Dry eyes, which are also referred to as dry eye syndrome (DES), dry eye disease (DED), ocular surface disease (OSD), dysfunctional tear syndrome (DTS), and keratoconjunctivitis sicca (KCS), rank among the most frequent reasons for consulting an eye specialist. According to the Tear Film and Ocular Surface Society (TFOS) Dry Eye Workshop II (DEWS II), the definition of dry eye is as follows: “Dry eye is a multifaceted condition of the ocular surface marked by a disruption of the tear film’s stability, along with ocular symptoms, where factors such as tear film instability and hyperosmolarity, inflammation and damage to the ocular surface, and neurosensory issues contribute to its causes.”
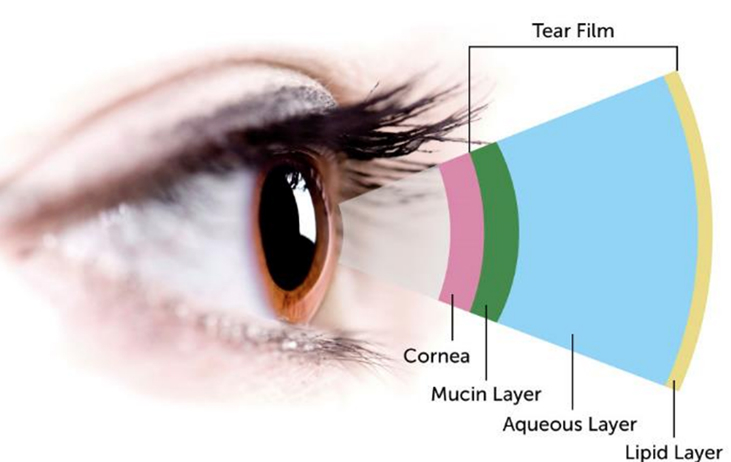
The most superficial layer; produced by the meibomian glands of the eyelids and functions to reduce the evaporation of tears
The middle layer and the thickest component of the tear film; produced by the lacrimal glands, located in the orbits and the accessory lacrimal glands (glands of Krause and Wolfring) in the conjunctiva. Aqueous fluid contains water, metabolites, electrolytes, peptides, proteins, etc.
Composed of mucins, or glycoproteins; predominantly produced by conjunctival goblet cells. Mucins enhance the spread of the tear film over the corneal epithelium through the regulation of surface tension.




DES and DED relate to a common ocular illness in which there is insufficient lubrication and moisture on the eye's surface. Numerous symptoms, such as dryness, irritation, burning, redness, and blurred vision, can be brought on by this illness. Even though the names are frequently used interchangeably, DED refers to a more comprehensive understanding of the disorder. It can be confusing because different medical practitioners and researchers use different terminologies.
This term is frequently used informally to refer to inadequate tear production or poor tear quality, which causes ocular pain and associated symptoms. Patients and medical professionals frequently use it to characterize the disease.
The multifaceted character of the ailment is better described by the more inclusive term DED. It recognizes that evaporative dry eye, aqueous deficit, and mixed etiologies are some underlying causes of dry eye, a complex and heterogeneous disease. DED covers a broader spectrum of clinical manifestations and causes.
DES is a broader term that emphasizes symptoms and a decline in tear quantity or quality rather than focusing on underlying causes in detail. DED acknowledges that the disorder has several facets and different subtypes. The 2017 TFOS DEWS II report offers a thorough categorization and in-depth explanation of dry eye illness. Inflammation, neurosensory abnormalities, and environmental triggers are just a few of the contributing elements the report considers when classifying DED into aqueous-deficient and evaporative subtypes.
Diagnostic procedures and therapies for DES and DED are comparable. A thorough eye exam that includes tests for tear film quality and quantity, a review of the ocular surface, and an evaluation of the patient’s stated symptoms is frequently required for diagnosis. Artificial tears, lubricating eye drops, dietary changes, anti inflammatory drugs, and, in extreme circumstances, procedures or operations may all be used as treatments. The underlying cause and severity of the condition determine the best course of action.

Over time, dry eye research has advanced, and our understanding of the condition has become more complex. In contemporary medical literature and research investigations, the term DED is used more frequently to reflect this thorough understanding. Inflammation, meibomian gland dysfunction, and the effect of the environment on the ocular surface have all been studied in recent DED studies. Researchers hope to advance patient care by utilizing the term DED to cover various contributing factors.
DED is usually classified into 2 major nonmutual exclusive etiology groups, which include evaporative dry eye and aqueous-deficiency dry eye. Excessive evaporation from the ocular surface can occur due to a reduced muco-aqueous component in the tear film, whereas aqueous deficiency is due to reduced production, usually based on underlying autoimmune or systemic conditions. Mixed cases of the 2 types can also be found in patients with dry eyes.
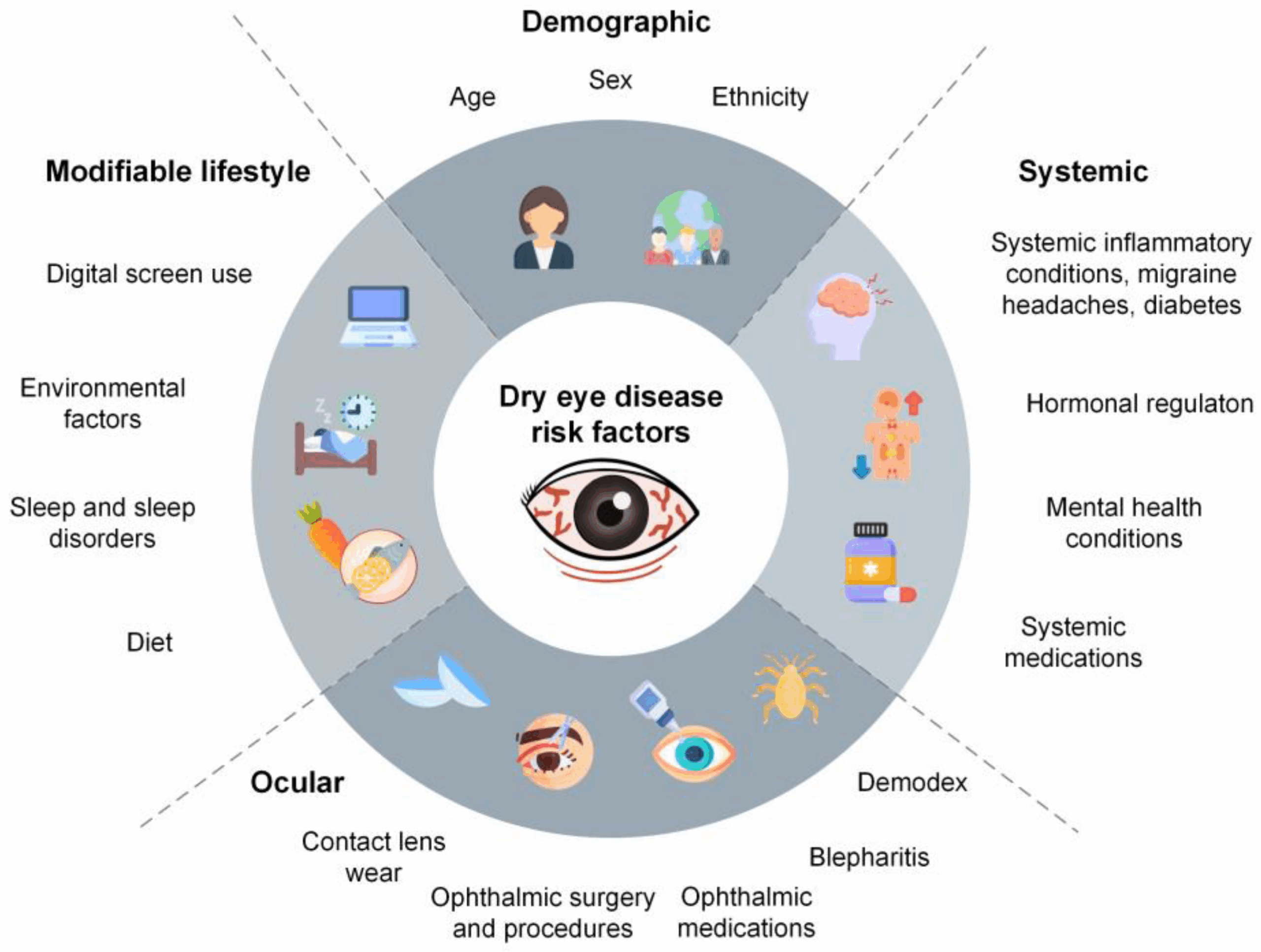
Numerous potential etiologies may contribute to the development of DED, and many cases may be multifactorial. These include local ocular factors, systemic diseases, sociodemographic factors, environmental conditions, and iatrogenic causes such as medications or surgeries. Potential causes or factors associated with dry eye include:
Dry eye is more common in women than men (due to female hormonal effects on the lacrimal and Meibomian glands and ocular surface) and has an increased prevalence with age. Studies have shown that female gender is a risk factor in developing dry eye, with a prevalence that ranges from 12% to 22%. The prevalence of DED worldwide varies depending on the diagnostic criteria employed, which ranges from approximately 5% to 50% in populationbased studies.
Dry eye has traditionally been classified into 2 categories: aqueous deficient and evaporative. These 2 categories, however, are not mutually exclusive, and numerous patients have a combination of these mechanisms of DED.

This category of dry eye is characterized by inadequate tear production. The predominant causes consist of Sjogren Syndrome (primary or secondary); diseases, inflammation, or dysfunction of the lacrimal gland; obstruction of the lacrimal gland; and systemic drugs (ie, decongestants, antihistamines, diuretics, beta-blockers, etc).

This category of dry eye is characterized by increased tear film evaporation and a deficiency in the lipid portion of the tear film. In this case, the quantity of tears produced is normal; however, the quality of tears causes excessive evaporation. This alteration is most frequently caused by meibomian gland dysfunction.

Meibomian glands line the eyelid margins and secrete oils that become the lipid layer of the tear film and reduce the evaporation of tears. Meibomian gland dysfunction may be caused Lacrimal gland by inadequate secretion due to atrophy, dropout of the glands, or obstruction of the gland orifices. Other major causes of increased tear evaporation include poor blinking (low rate, incomplete lid closure), lid aperture disorders, vitamin A deficiency, contact lens use, and environmental factors (low humidity, high airflow).
A hallmark of DED is hyperosmolarity of the tear film, which may damage the ocular surface directly or indirectly by inciting inflammation, tear film instability, epitheliopathy, and ocular surface neurosensory abnormality. The normal osmolarity of the tear film is usually less than 300 mOsm/L, which has been reported to be as high as 360 mOsm/L in patients with DED.
Hyperosmolarity of the tear film leads to a cascade of signaling events that releases inflammatory mediators (ie, tumor necrosis factor, cytokines, alarmins, interleukin 1 and 6, etc.). It leads to damage to the ocular surface, which may further decrease tear film stability, leading to self-perpetuation of the disease in a vicious cycle. Apart from hyperosmolarity, other factors may initiate this pathologic cycle, including ocular surface inflammation caused by conditions such as allergic eye disease, topical preservative toxicity, or xerophthalmia.

DED may lead to a number of symptoms, ranging from mild to severe:




There is no single gold standard sign or symptom for diagnosing DED. Evaluation of symptoms and signs of DED is recommended, as signs may be present without symptoms and vice-versa.
A verbal history allows the nonscripted elicitation of dry eye symptoms. In addition, many questionnaires have been developed to screen for symptoms of DED. Using a validated questionnaire allows accurate quantification of symptoms as a screening tool and monitoring for progression and response to treatments. Several questionnaires exist, such as the Ocular Surface Disease Index (OSDI),Dry Eye Questionnaire (DEQ-5), and Symptoms Analysis in Dry Eye (SANDE), and others, which may help assess dry eye symptoms. Many questionnaires also include questions about subjective visual function or disturbances that may be attributable to dry eye.
Tear film breakup time (TBUT) is the interval between a complete blink and the first break in the tear film. This is most often performed in the clinic using a slit lamp microscope after instilling sodium fluorescein stain to enhance the visibility of the tear film. A cutoff of fewer than 10 seconds for the appearance of a patch in the tear film is often considered consistent with DED. Alternatively, a non-invasive tear breakup time can be measured without fluorescein using instrumentation that evaluates the reflections of patterns or rings from the tear film or interferometry to assess for the appearance of discontinuity of the lipid layer after a blink. Studies have shown corneal hyperalgesia in eyes with a shorter TBUT.
A TBUT greater than 10 seconds is generally considered normal, indicating a stable tear film.
A TBUT less than 10 seconds may suggest evaporative dry eye, and values less than 5 seconds are strongly indicative of significant dry eye disease.
TBUT is a common diagnostic tool for evaluating dry eye and monitoring its effectiveness
Assessment of the tear meniscus is performed at the slit lamp by judging the inferior tear film meniscus height. This technique is simple to perform but is subject to poor intervisit repeatability. Instrumentation has been developed for more objective measurement of the tear film meniscus but is not currently widely available in most clinics.
A Schirmer paper strip is folded at the notch with the shorter end hooked over the lateral lid margin to avoid cornea irritation while the patient rests with closed eyes. The Schirmer I test is performed without topical anesthetic to measure basic and reflex tearing with less than 5 to 10 mm (depending on cutoff used) of wetting after 5 minutes of diagnostic of aqueous deficiency. Alternatively, a topical anesthetic can be administered. Then, residual fluid blotted from the inferior fornix before performing testing to measure basic secretion with less than 5 to 10 mm of wetting is considered diagnostic for aqueous deficiency.
Like Schirmer testing, a cotton thread dyed with phenol red is hooked over the temporal eyelid into the sulcus for 15 seconds while the patient rests with closed eyes. When wet, the thread turns red with cutoff values ranging from less than 10 to 20 mm used clinically.
Fluorescein staining allows the assessment of corneal damage. A minimal volume of fluorescein is instilled into the tear film with optimal viewing 1 to 3 minutes later. Greater than five spots of staining are considered positive results, with various grading scales, such as the Oxford grading scale, also used.
Lissamine allows the assessment of conjunctival and lid margin damage and, to a lesser extent, corneal damage. Greater than nine spots is a positive result. Lid wiper epitheliopathy, or staining of the lid margin, can be performed with a positive result as 2 mm or more staining in length or greater than 25% in sagittal width.
Conjunctival redness, or hyperemia, is not specific to DED as this may result from any stimulus that results in conjunctivitis, including infective, allergic, chemical, or mechanical etiologies. Grading is generally determined subjectively by slit lamp examination, although some devices with automated grading or digital photography can also be used.
Elevated osmolarity and increased variability of osmolarity of the tears are characteristics of DED. Osmolarity values typically increase with disease severity. Various cutoff values have been reported, with 308 mOsm/L used as a threshold to diagnose mild-to-moderate disease, whereas 316 mOsm/L has been used as a cutoff for more severe disease. Studies have shown that high osmolarity levels can lead to proinflammatory effects on the ocular surface, with the secretion of inflammatory cytokines and metalloproteinases that can cause chronic epithelium dysfunction and induce apoptosis.
These proteases are found in the tears of individuals with dry eyes. Matrix metalloproteinase-9 (MMP-9) levels can be tested using a point-of-care test.
Evaluation of the eyelids is a crucial part of the evaluation to determine any factors contributing to DED. The evaluation includes assessment for anterior blepharitis and demodex blepharitis, which are frequent comorbidities of DED.
The portion of conjunctiva along the lid margin that contacts the ocular surface to spread tears has been termed the “lid wiper.” Lid wiper epitheliopathy, or staining of the lid wiper with fluorescein or lissamine green, may be seen more commonly in individuals with DED, presumably due to increased friction between the lid and ocular surface.
The evaluation of the meibomian gland structure can be performed with meibography Although the outline of meibomian glands can be seen at the slit lamp or with a penlight by transilluminating the everted eyelid, enhanced visualization is obtained using infrared imaging systems to perform meibography. Inspection of the meibomian gland orifices along the eyelid margin can be performed to detect external obstructions of orifices. Meibomian gland function can be assessed by evaluating meibum quantity, quality, and expressibility. Expressibility is assessed by applying digital pressure along the eyelid margin with a clear meibum easily expressed from the normal eyelid. Themeibum is turbid or viscous in meibomian gland dysfunction and is not easily expressed.
Incomplete blinking and nocturnal lagophthalmos can result in DED. Blink assessment can be performed with or without a microscope or video recording equipment. Lagophthalmos can be estimated by having the patient gently close their eyes and assessing for incomplete closure.
Evaluation for Systemic Disease
Numerous systemic diseases may cause DED, particularly primary Sjogren syndrome and secondary Sjogren syndrome caused by other autoimmune conditions such as rheumatoid arthritis, lupus, progressive systemic sclerosis, and dermatomyositis. Other systemic abnormalities such as Parkinson’s disease, androgen deficiency, thyroid disease, and diabetes have also been associated with DED.
Evaluation for systemic disease causing secondary dry eye may be warranted if an underlying condition is suspected. A review of systems is indicated to screen for underlying systemic diseases. Sjogren syndrome may also involve the salivary glands leading to dry mouth and predisposing to periodontal disease, and other mucous membranes may be affected, such as vaginal, gastric, and respiratory mucosae. Laboratory testing for Sjogren syndrome (antibodies to Ro/SS-A or La/SS-B), rheumatoid factor, and antinuclear antibodies. Referral to a rheumatologist may be indicated, and some cases of Sjogren syndrome may require a salivary gland biopsy by an oral surgeon.
Treatment of DES is performed in a step-wise approach that may vary depending on the severity of the disease.
Initial approaches include:
Therapy aims to decrease signs and symptoms, restore ocular surface homeostasis, and enhance quality of life.

Complications from DED range from mild to severe. Mild-to-moderate DED causes symptoms detailed above, including ocular irritation or visual disturbances. More severe diseases can result in corneal complications, including infectious keratitis, ulceration, and scarring, which may cause subsequent loss of vision. Although causation has not been established, several nonocular associations exist with DED, including depression, sleep and mood disorders, dyslipidemia, and migraine headaches.
In cases of primary or secondary Sjogren syndrome, treatment of the underlying disorder is often needed to treat the ocular manifestations adequately. Early identification and management of patients with dry eyes are imperative in reducing ocular symptoms and irreversible complications. Caring for patients with dry eyes necessitates a collaborative approach among healthcare professionals to ensure patient-centered care and improve overall outcomes. Health professionals involved in the care of these patients should possess the essential clinical skills and knowledge to diagnose and manage dry eye syndrome accurately.
The primary care provider, ophthalmic nurse, and pharmacist should educate patients on the prevention and basic treatments of dry eyes by limiting screen time, blinking often, using artificial tears, and keeping the home environment cool and moist. Eye care providers



This unique treatment helps treat eyelid redness, promote healthy gland function, and relieve dry eye symptoms

This is a non-invasive, in-clinic procedure designed to treat Meibomian Gland Dysfunction (MGD), one of the most common causes of dry eye. The treatment uses a combination of controlled heat and gentle pulsatile pressure.

Low Level Light Therapy (LLLT) is a powerful and unique treatment that counteracts the obstruction or malfunction of the Meibomian glands by unclogging the oils needed to keep eyes healthy, moisturized and comfortable.

Blepharitis is a common and persistent condition that causes inflammation of your eyelids.
Once your condition is fully diagnosed, our doctors can create an effective treatment plan to manage your blepharitis condition.

Amniotic Membranes are a super simple and effective treatment for certain cases of dry eye.
It works like a bandage to protect the surface of the eye while it heals. It also significantly reduces pain caused by friction of the eyelids.
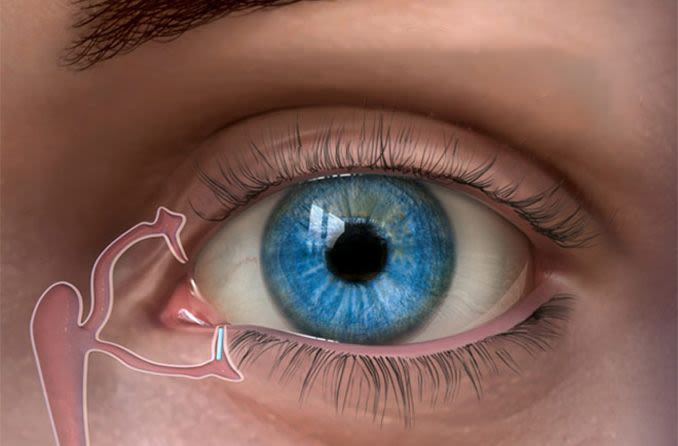
Punctal Plug treatment is designed to help increase moisture in the surface of your eyes.
Punctal plugs are tiny semi-permanent or dissolvable devices that can be inserted into tear ducts to block drainage.
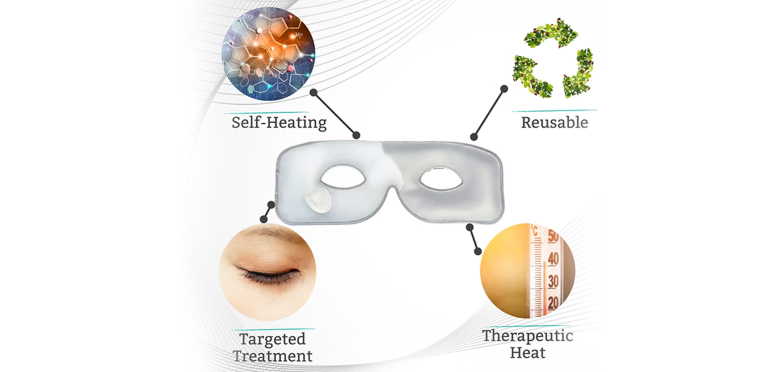
Blinking serves as an instinctive method to hydrate your eyes. The thermal mask for open eyes warms up and releases the oils found in your eyelids, rejuvenating your tears. When this is paired with the natural cadence of blinking, it speeds up the process of treatment, comfort, and effectiveness. Furthermore, with this groundbreaking solution, you can take care of your eyes while enjoying a book, completing household tasks, or sending work-related emails – effortlessly integrating eye care into your everyday life.

Many individuals suffering from dry eye disease can benefit from prescription medications, particularly preservative-free eye drops. These formulations not only provide symptomatic relief but also address the underlying causes of the condition, offering a more comprehensive approach to treatment.